Background and objectives
The current National Institute for Health and Care Research Blood and Transplant Research Unit in Organ Donation and Transplantation (NIHR BTRU in ODT) builds on the success of its predecessor, the 2015–2022 NIHR BTRU in ODT. This was also a partnership between the University of Cambridge, Newcastle University and NHS Blood and Transplant (NHSBT). The unit ran from 1 October 2015 to 31 March 2022 and its strategic aims were to increase the number of suitable organ donors and to improve the long-term results of solid organ transplantation.
Unit structure
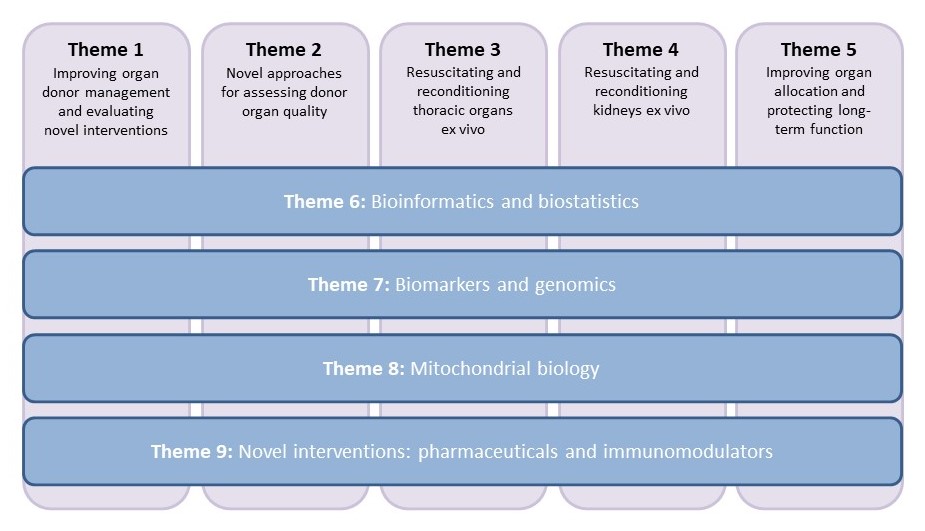
Research was carried out under five main research themes and four cross-cutting themes:
Major research findings
1. Normothermic regional perfusion (NRP) involves using a machine to recirculate a deceased donor’s blood through the thoracic and abdominal organs after death. The NRP machine warms the blood and adds oxygen to it, which reduces organ damage caused by cold storage. BTRU research led to the introduction of NRP as the UK standard of care for liver transplantation from circulatory death donors (DCDs). NRP doubled the utilisation rate of DCD livers (28% to 55%) and reduced damage to the ducts that drain bile from the liver from 20% to 2%.
2. Normothermic machine perfusion (NMP) is a related technique that circulates warmed, oxygen-rich blood through donor organs after they have been removed from the donor (ex vivo). Our research underpinned the widespread introduction of clinical NMP for lungs, liver and kidneys. This included the world’s first multicentre clinical trial of NMP in 338 DCD kidney transplants. NMP was used to identify changes in the genes in transplant organs that predict the outcomes of liver and kidney transplantation. NMP also enabled delivery of novel therapies to discard human organs including the first-in-human study of stems cells in kidneys. Stem cells can develop into any type of cell in the human body and have the potential to repair injured cells in transplants. NMP of the lungs identified an inflammatory molecule (called interleukin 1β) that predicts whether lungs will work after transplantation.
3. The NHSBT national database was used to demonstrate the safety of transplanting organs from high-risk donors who were previously excluded (hepatitis C and HIV, meningitis/encephalitis, death from ligature asphyxiation). This was an important change in national healthcare policy.
4. The development of antibodies against transplants is one of the commonest causes of transplant failure but it is difficult to know which antibodies are important. BTRU research designed a new laboratory method that allows measurement of the level of antibodies and how strongly they bind to transplant cells (stickiness). This allows us to ignore unimportant antibodies that previously prevented some patients from being transplanted.
5. BTRU researchers were commissioned by DHSC via NIHR to perform a systematic review and evidence synthesis in the factors influencing organ donation rates in Black, Asian and Minority Ethnic communities and conducted two workshops, culminating in a report and policy statement.
Outputs, impacts and dissemination
The BTRU leveraged an additional £19M in external grant funding including awards from the NIHR, the Medical Research Council and Wellcome. The unit published 72 papers in peer-reviewed journals (including Nature and Science). BTRU research fellows presented >80 papers to international/national meetings and were awarded the da Vinci Medal (European Society of Transplantation), the Medawar Medal and Roy Calne Prize (British Transplantation Society) and the Patey Prize (Surgical Research Society). Twelve of our research fellows were awarded a PhD.
The future
The 2015–2022 NIHR BTRU in ODT delivered effective bidirectional research between scientists and clinical researchers that has informed changes in national transplant policy and clinical practice. The unit met its strategic aims of increasing the number of suitable organ donors and improving the long-term results of solid organ transplantation. The universities of Newcastle and Cambridge were successfully awarded NIHR BTRU status again in open competition in 2021. The new unit will build on the considerable success of the 2015–2022 BTRU in ODT to deliver world-class fundamental, clinical translational and applied health research.

